My Report to the President
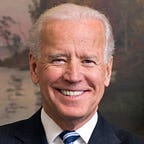
Dear Mr. President:
As you walked Jill and me out into the Rose Garden almost exactly a year ago and I announced that I would not run for president, I said in my remarks that I had only one regret — that I wouldn’t be the president who presided over the end of cancer as we know it. I said it because I believe it’s possible.
As every family facing cancer does, Jill and I and our family learned as much as we could about the cancer our Beau fought from the diagnosis to the very end.
We had access to the world’s best nurses, physicians, and researchers. And the more time we spent with them, the more we understood that even if we couldn’t save our son, the science, medicine, and technology are progressing faster than ever to save countless other sons and daughters. There’s a recognition that the cancer system of the 20th Century must be reimagined for the 21st Century to match the breakthroughs creating an inflection point in this fight.
A few months later during your State of the Union Address, to my surprise and with my gratitude, you asked me to lead a new “Cancer Moonshot” to inject a sense of urgency to seize this moment. You followed up with a Presidential Memorandum putting me in charge of a new Cancer Moonshot Task Force to unite and marshal every resource of the Federal government to achieve the Moonshot’s mission — to make a decade of progress in five years in preventing, diagnosing, and treating cancer. You also created a Blue Ribbon Panel of top experts and advocates from a range of disciplines that’s already identified the scientific priorities to change the many faces of cancer.
And with the charge you gave me, Jill and I also traveled around the country and the world, meeting with thousands of cancer patients and their families, physicians, researchers, philanthropists, technology leaders, heads of states, and even Pope Francis. We sought to better understand and break down the silos and stovepipes that prevent sharing of information and impede advances in cancer research and treatment, while building a focused and coordinated effort at home and abroad.
This report to you outlines what we’ve accomplished in year one and lays out the roadmap for the continuation of a five-year plan. And it’s also a report to the American people, sharing the story of the spirit of discovery that defines this country and that gives me every confidence that we can do this.
As you know very personally, cancer touches us all in some way and at some point.
Everywhere I go, people share their stories of heartbreak and hope. And every day, I’m reminded the Cancer Moonshot is bigger than just a single person. It carries the hopes and dreams of millions of people who are praying that we succeed, praying for hope, praying for time — not someday, but now. It’s all of us coming together, as you’ve said, for the loved ones we’ve lost and the ones we can save.
Joe
Launching the Cancer Moonshot
The mission of this Cancer Moonshot is not to start another war on cancer, but to win the one President Nixon declared in 1971. At that time, we didn’t have the army organized, didn’t have the military intelligence to know the enemy well, and therefore didn’t have the comprehensive strategy needed to launch a successful attack — now we do. Because of the progress over the last 45 years we have an army of researchers and oncologists, the powerful technologies and weapons, and immense public support and commitment to action.
Immediately following the launch of the Cancer Moonshot, I engaged in an extensive “listening tour”, meeting with patients and their families, physicians, researchers, and other experts to gain an even better understanding of what challenges impede advances in cancer research and treatment, and what opportunities could be realized with a focused and coordinated effort. I visited many of the major nerve centers in the fight against cancer to gain as much information as I possibly could in order to meet our goal and sense of urgency.
I learned there is consensus that in the cancer fight, we have reached an inflection point, and there is good reason to have hope. Let me explain what I mean by that:
- There is more collaboration across research disciplines than ever before, and this is needed to solve the complexity of a challenge like cancer. Five years ago, oncologists weren’t routinely working closely with immunologists, virologists, geneticists, chemical engineers, and others — now they are.
- Because of technological advances, researchers are now able to analyze cancer genes and proteins, along with other genes in the body, putting us closer than ever before to understanding what causes cancer and how to attack a particular cancer.
- Using this improved understanding of cancer biology, we can now target and treat cancer cells with therapies that boost the immune system, that use low doses and new forms of radiation, and more targeted chemotherapy. Many of these new treatments are effective at killing cancer cells while doing less damage to healthy cells, advances could eventually transform many types of cancer that are currently hard to treat such as liver cancer, brain cancer, and pancreatic cancer into chronic, manageable diseases.
- Everywhere I travelled, I was told that data are key, and we have an unprecedented amount and diversity of data being generated daily through genomics, family history records, lifestyle measurements, and treatment outcomes; with this data we can find new patterns of causes, earlier signs of cancer, and successful treatments of cancer.
- We now have the capability to realize the promise of all of these data because of advances in super computing power. Researchers can analyze enormously complex and large amounts of data to find answers we couldn’t just five years ago.
- And we have more Americans than ever before covered by health insurance, through the Affordable Care Act (ACA). As a result of the ACA, a diagnosis of cancer doesn’t mean you lose your insurance if you change plans because you have a pre-existing condition. And it means more Americans can take advantage of prevention tools and early screening measures leading to earlier detection of cancer that results, in many cases, in better outcomes.
Challenges and Opportunities
While there is great promise and reason to be optimistic, we must meet this opportunity with action. There are remaining barriers that must be addressed as part of the Cancer Moonshot. From my interactions it was increasingly clear, that there is a lack of coordination among efforts, a failure to share information both rapidly and effectively, and an antiquated culture of research and funding. Specific barriers include:
- Incentive structures that encourage and reward individual success rather than cross-discipline and cross-sector collaboration, making it even harder to pursue team science which can lead to new answers and new solutions.
- Poor retention and recruitment in cancer clinical research trials, and insufficient dissemination of successful strategies for engaging participants as partners in research. These inefficiencies can lead to costly hurdles in conducting successful trials and unacceptable delays in getting new treatments to patients.
- A lack of open access and rapid sharing of research data and results allowing researchers to build on each other’s successes — and failures — to make new discoveries faster.
- Hurdles surrounding the sharing of medical records that offer no additional level of protections for patients.
- Insufficient collaboration around, and utilization of, technological capabilities to harness the vast amounts of data within our electronic health records to improve cancer prevention, diagnosis, treatment, and care.
- Slow dissemination of “cancer center knowledge” — new discoveries, new diagnostics and screening measures, new clinical trials, and new treatments — equitably throughout the population, especially in community practices across the United States.
But I am convinced these barriers are not insurmountable. And, through the work of this Administration and the efforts of Cancer Moonshot, we are already making progress.
Progress on the Cancer Moonshot
Cancer Moonshot Task Force
I have been amazed and impressed by the response to this new effort to end cancer as we as know it, this Cancer Moonshot, with individuals and organizations, agencies, and nations stepping up to take on these challenges.
Mr. President, under the Cancer Moonshot Task Force you created, my first order of business was to infuse a new sense of urgency within the Federal government, to bring together department and agency leaders to unite their focus in removing unnecessary barriers and launching new programs and collaborations. I am pleased to announce the progress we have made in this short time.
For instance:
To share research results and data faster, NIH launched a new partnership, to bring together drug companies, major cancer research centers, foundations, and philanthropies to collaborate on early stage research — i.e. the basic biology of cancer — and to share all of the data with everyone. So instead of 20 companies each studying the same thing and not sharing the results, they’ll be able to see each other’s findings and build upon the results more quickly. The drug companies have realized this is in their interest and more are signing up.
To encourage a greater sense of collaboration, NCI, in June, launched a Drug Formulary — a new public-private partnership with 20–30 pharmaceutical and biotechnology companies that allow researchers to more easily license and test their existing drugs for new combinations that could be effective against different types of cancer. Trials using combination therapies (therapies using more than one drug), which potentially improve the likelihood of curing a particular cancer, can now be streamlined to move more quickly.
To support innovation, the U.S. Patent and Trademark Office (USPTO) launched a free and accelerated pilot program that aims to cut in half the time it takes to review patent applications in select fields of cancer therapy, from an average of about two years to less than 12 months. The USPTO also opened up their application data and challenged innovators to develop new ways to study gaps and great areas of promise in cancer research based on patent filings.
To apply 21st century technology to biological questions, the U.S. Department of Veteran’s Affairs (VA) and the Department of Energy (DOE) have partnered to apply the most powerful computational assets at the DOE’s National Labs to over half a million veterans’ records from one of the world’s largest research cohorts — the Million Veteran Program — a cornerstone of your Precision Medicine Initiative. The collaboration is poised to drive new understanding of cancer and new patterns in effective treatments as part of the Cancer Moonshot.
To streamline and coordinate review of cancer products, the U.S. Food and Drug Administration (FDA) created an Oncology Center of Excellence (OCE) to maximize the availability of oncology expertise and review on cancer-related applications. The OCE unites cancer product regulatory review to enhance coordination and leverage the combined skills and clinical expertise across FDA centers to accelerate bringing new, safe therapies to market.
To implement successful prevention measures, the Centers for Disease Control and Prevention (CDC) is advancing its efforts to promote cancer vaccines as a safe and effective strategy for combatting various types of cancers. This centers on working to increase HPV vaccination rates by raising awareness about the importance of vaccinating males and females ages 11–12, and maximizing access to and opportunities for vaccination.
And to increase the ability for patients to participate in clinical research, the NCI has adopted a new “dashboard” that makes it easier for patients and doctors to search for clinical trials. This dashboard was created by the Presidential Innovation Fellows in partnership with the NCI to maximize the user experience when they go to trials.cancer.gov.
As part of this work, the Task Force identified ways in which the Cancer Moonshot could build on this Administrations related efforts, including our push to increase biomedical research funding and the launch of programs like the Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative and the Precision Medicine Initiative (PMI).
Private Sector Engagement and Action
But, Mr. President, we all know the Federal government cannot do this alone.
As part of igniting the Cancer Moonshot national conversation and call to action, on June 29, 2016, I brought together nearly 400 cancer researchers, oncologists, nurses, patients, their families, advocates and others in Washington, D.C. for a Cancer Moonshot Summit. Over 7,000 more convened at hospitals, community care centers, businesses, and in family rooms at more than 300 local summits across all 50 states, Puerto Rico, and Guam.
The goal of this Summit was to ignite a national — and even international — conversation to fundamentally change the trajectory of progress in cancer prevention, diagnosis, treatment, and care to make a decade’s worth of progress in half the time. Including the Summit and the release of this report, we will have announced 54 new private sector actions and collaborations, in addition to new Federal efforts, to make progress on Cancer Moonshot goals.
Responses to our call to action have emerged from across the country, with organizations committing to make a difference as part of the Cancer Moonshot — from the American Cancer Society setting the goal of doubling their research investment over the next five years, to the Alex’s Lemonade Stand Foundation doubling its investment in childhood cancer research projects and family services over the next five years, to ride-sharing services like Uber and Lyft offering reliable and affordable travel to treatments and appointments for patients who need it.
Others have stepped up, as well, for example, Deloitte’s “Conquering Cancer” XPRIZE focused on simplified early detection technologies was certified by XPRIZE as ‘ready for launch’ at the Visioneers 2016 Summit. This competition will bring new minds and teams together to develop innovative solutions for early detection. And, Cancer Support Community (CSC), a world-wide network of community-based and online patient support, launched the Frankly Speaking About Cancer Clinical Trials program, to reach at least half a million patients with an education series devoted to dispelling common myths and building awareness among patients and caregivers about the importance of clinical trials.
And in communities across the country, local governments and cancer centers are taking up the challenge. For example, the MedStar Washington Hospital Center, Washington Cancer Institute, launched a “Colon Cancer Prevention in the Neighborhood” Program to take place over the next year. The goal is to deploy a team of healthcare professionals to work with neighborhoods in Washington, D.C. to build community-based partnerships to deliver colon cancer education, perform risk assessments, and distribute colon cancer tests to return for free testing for over 1,400 residents. And Mercy Hospital has answered the call by doubling the number of free mammograms, diagnostic procedures and breast health education programs to the uninsured and underinsured women in the Oklahoma City community. Through Project Early Detection, more than 1,100 women will be offered access to breast health care.
The Cancer Moonshot has spurred new private partnerships and collaborations. For example:
- Representatives from government, academic, pharmaceutical and diagnostic companies have agreed to accelerate the development of an open database for blood profiling diagnostic technologies for patient benefit.
- Earlier this year, I was in Chicago for the launch of the NCI’s Genomic Data Commons — a platform built by the University of Chicago for the NCI and also part of your Precision Medicine Initiative. With this new national resource, researchers can freely access raw genomic and clinical data for more than 32,000 patients, with patient privacy and data security safeguards in place, and more records to follow. Increasing the pool of researchers who can access data — and decreasing the time it takes for them to review and find new patterns in that data — is critical to speeding up the development of lifesaving treatments for patients. And we know that people are finding this resource valuable, with more than 5 million users and more than 50 million data downloads worldwide since June.
- Because of the Cancer Moonshot call for greater prevention efforts, there’s now a collaboration between George Washington University and the Case Comprehensive Cancer Center focused specifically on tobacco cessation and cancer prevention and screenings. Washington, D.C. and Cleveland have higher than the national average smoking rates. This new program uses social media and digital monitoring technologies to help people adopt healthier life styles.
- IBM, the U.S. Department of Defense (DoD, Walter Reed Murtha Cancer Center) and VA have launched a public-private partnership to help doctors scale access to precision medicine for 10,000 American Veterans with cancer over the next two years. VA cancer patients will have DNA sequenced at the Murtha Cancer Center, and IBM will provide Watson for Genomics, which has been trained for genomic analysis, to VA doctors to help them identify the likely cancer-causing mutations and treatment options that target those specific mutations — a data-intensive process that has been time consuming and difficult to scale in the past.
Earlier this year, I was asked by the Vatican to keynote its conference on regenerative medicine and talk about the Cancer Moonshot. At the conference, I outlined five pillars for an international commitment to change the culture of our global fight against cancer.
- Increase global focus on cancer prevention, and treatment access and affordability.
- Raise the international response to cancer with the same urgency we bring to infectious disease threats.
- Increase research and patient data sharing — among researchers, institutions, foundations, and nations.
- Support international standardization of data and bio-repositories, so records can be easily shared and compared with data from medical centers across the world.
- Increase worldwide government investment in cancer research.
During the United Nations General Assembly meeting in September, I announced three major steps that go to the heart of these pillars and demonstrate the progress we have made this year.
First, the United States executed ten new Memoranda of Understanding (MOUs) and commitments to nine nations that will support greater international cancer research and care. For example, seven of these MOUs — with institutions in Canada, China, Germany, Switzerland, Taiwan, Japan, and the Republic of Korea — focus on the emerging field of proteogenomics, which studies the relationship between genes and proteins and, in this case, their role in cancer.
Second, we announced NCI investment in the creation of regional hubs to help reduce disparities in cancer research — in parts of the world that are under-resourced to support research and programs to deliver better cancer prevention, diagnosis, and care.
Third, the U.S. Department of State has strengthened U.S. bilateral science and technology engagements — engagements the United States has with more than 70 countries — to support the Cancer Moonshot and these international guideposts.
Cancer Moonshot the Road Ahead: Strategic Plan
I am enthusiastic about what can be accomplished when we are united in this fight. We have demonstrated what can be achieved and what is possible. We must continue to support the charge, as so much more is left to do to truly improve patient outcomes. Moving forward, we must focus our efforts in a few strategic areas.
Realign the Incentives in the Research System
Mr. President, one of the most common things I hear is that we need to realign incentives in our cancer research enterprise. This is a message I took up when I addressed 5,000 of our nation’s top cancer researchers at a major conference in New Orleans.
Our cancer system as we know it was established in 1971, when President Nixon signed the National Cancer Act, initiating the first National Cancer Program, the President’s Cancer Panel and the National Cancer Advisory Board. But it is time to re-imagine a cancer enterprise for the 21st century.
The central role of government in funding cancer research requires us to reinvent our approach periodically to match the times — and the opportunity, and that time is now. System reform and the establishment of new incentives are essential aspects of the Cancer Moonshot to ensure that scientific progress can accelerate at the pace needed to achieve our goal. I am working across the Federal government and with the private, academic, and philanthropic sectors to identify areas in which system change could lead to meaningful and sustained impact for patients.
Areas for further action include implementing strategies for spurring innovative cancer research, particularly those supported by the NCI by:
- Creating new funding mechanisms for supporting high-risk/high-reward research;
- Implementing pilot programs to accelerate receipt, review, and funding of meritorious research proposals;
- Incentivizing public access to publications at the time of publication; and
- Reforming and revitalizing the NCI intramural research program (its cadre of Federal scientists) as a center of excellence for addressing emerging scientific opportunities or grand challenges in public health, including cancer.
Enhance Prevention and Screening Efforts
By some estimates, at least 50 percent of cancers can be prevented. Prevention falls into three major categories of action: (1) personal actions of an individual, such as living a healthy lifestyle and avoiding cancer risk behaviors, such as smoking; (2) responsibilities of a government, such as reducing carcinogens in the air, ensuring the availability of clean drinking water, and protecting its citizens from known toxins; and (3) technology and medical advances that enable us to prevent and detect cancer earlier.
While there is progress to make across all of these areas, there is great potential for new breakthroughs in the last category. There is new hope, as emerging technologies are paving the way for new non-invasive and mobile imaging techniques and new genetic “markers” to identify those at risk for developing cancer long before the cancer progresses.
We must continue to invest in research to understand cancer prevention and in new, effective, methods to reach individuals and communities with prevention tools and education, recommended vaccinations, and early screening.
Engage Patients as Partners in Research
While the challenges around patient data in the healthcare system are not trivial to overcome, there are some known steps that we must take. Ultimately, we have to build a network — centered on the patient–that makes data accessible, shareable, and meaningful. And we must advance a modern, interoperable electronic health ecosystem, with patient access and sharing capabilities between clinical care providers and research. This Administration has made critical improvements in this area, such as clarifying patients’ rights to access their health information and overseeing the adoption of electronic health records in clinical care. But there is more to do.
To realize this, we should provide all patients the ability to easily access, reconcile, and share their health information in ways that work for them, so that they can make informed decisions about their healthcare. These steps will also enable patients, especially those who have multiple providers, improved care coordination and delivery since they would be able to bring their records with them — or have them sent in advance — as they move between doctors and practices. Importantly, this system must respect and protect patients’ preferences for privacy, and allow them to use their data as they choose.
For example, additional steps could include:
- Coordinating pilots with providers and electronic health record vendors to make it easier for cancer patients to share copies of their records for their own care coordination or data donation to research;
- Ensuring individuals understand their rights to direct their data where they want it to go, helping put them in control of their health and care;
- Creating the ability for patients to have all of their information in one accessible location. At the patient’s direction, clinical information would automatically be sent to this location and patients would be able to easily share their data from the location with providers, family or researchers.
- Implementing a rapid standards adoption process for medical data similar to the standards used for clinical data; and
- Promoting the adoption of interoperable electronic health system through effective incentives and contracting requirements.
Expand Access to Care
We must ensure that advances in research and care benefit all segments of society and that our commitment to diversity in cancer clinical trials reflects the critical importance of ensuring that access is equitable. We must provide better support to patients so that gains in precision oncology are matched by improvements in individualized treatment. And we must support the delivery of quality oncology care to every cancer patient regardless of socioeconomic factors, rarity of illness, age, or geographic limitations in healthcare access.
To realize this we could:
- Engage more communities in cancer research to develop better genomic, environmental and treatment response data about cancer in underserved and underrepresented populations. This includes, exploring ways to address the challenges that limit minority participation in clinical research (e.g., social determinants of health), and ensure that historically underrepresented communities are involved in the planning, design, and implementation of clinical trials.
- Allocate Federal and private funds to support the frontline efforts of community clinics in increasing health literacy among all populations, involving community groups to promote the value of prevention, early screening, and cancer clinical trial participation, and optimizing medical interactions to raise awareness and recruit potential participants.
- Promote best practices for both cancer centers and community practices that effectively and sustainably address cancer disparities.
- Identify pathways for disseminating clinical advances to community oncologists and their patients.
- Endorse public-private partnerships that innovate drug development for rare and pediatric cancers.
- Support research in cancer survivorship, and identifying best practices in clinical management of the patient in remission.
Create New Financial Models to Improve Development of and Access to New Therapies While Addressing the Issue of Rising Drug Prices
We must create new financial mechanisms to leverage private investment to advance new cancer prevention methods, diagnostics, and therapies. We must ensure that insurance coverage decisions are rooted in data, including medical efficacy, clinical effectiveness, and ultimately health outcomes. We must improve pathways and opportunities for medically uninsured and underinsured cancer patients to obtain preventive measures and life-saving treatments. And we must create incentives through legislative, regulatory, and reimbursement venues to enhance cooperation and collaboration across the industry as early as possible in the development cycle, especially in the development of new products and treatments for rare and pediatric cancers.
To realize this, we could:
- Convene finance and philanthropic leaders to spur the development of additional private investment models in alignment with the Cancer Moonshot.
- Explore options for the Federal government to establish a bond or fund to leverage taxpayer dollars to bring compounds and devices across the “valley of death” between foundational research and applications to healthcare delivery.
We must address the escalating costs of cancer care. Lifesaving drugs are expensive to develop and create great value to individuals and society. It is important that we continue to incentivize investment in this area, and that the lifecycle of drug development can be sustained. But price increases without any market justification have become the norm not the exception in the pharmaceutical industry and pose a problem for payers and patients. Often price increases benefit the middlemen while disadvantaging patients. Co-pays required by insurance companies and pharmacy benefit managers are often more expensive for the most efficacious drugs than for less effective drugs, further distorting the system.
To address the complexity of drug pricing and the delivery system for drugs:
- We need to have a national conversation, including biopharmaceutical companies, insurers, pharmacy benefit managers, Congress and patient advocacy groups, about drug pricing to ensure that high-quality treatments are financially accessible to all patients, including vulnerable and medically-underserved populations and that we have a more rational system to price and pay for new medications.
Concluding Thoughts
Mr. President, earlier this year I spoke at Rice University, nearly fifty years to the day from when President Kennedy spoke about the Nation’s first moonshot, when he said,
“We choose to go to the moon in this decade and do the other things,
not because they are easy,
but because they are hard,
because that goal will serve to organize and measure the best of our energies and skills, because that challenge is one that we are willing to accept,
one we are unwilling to postpone, and
one which we intend to win, and the others, too.”
That’s where we are today in our Cancer Moonshot. While there is only one moon, there are more than 200 distinct kinds of cancer — not all susceptible to the same detection strategy or treatment, but each requiring all of us to be unwilling to postpone.
There are thousands of brilliant researchers spending nights and weekends in their labs looking for the next breakthrough. Countless patients full of courage, hoping they can return to their lives and their families, or asking for just three more months to walk a daughter down the aisle. Brave family members starting foundations, not just to remember, but to honor their husband, wife, brother, sister, son, or daughter. Companies and entrepreneurs developing cures and technologies the right way for the right reason. Everyone from philanthropists pouring their own money into the fight to the little girl and her lemonade stand doing her part to help her classmate. And it’s the Congress stepping up for massive increases in funding for cancer research and care.
The Cancer Moonshot is a movement that lives in communities across the United States and the world — and it will live long after we leave office. Mr. President, we can’t afford for it not to, because the need is too great and the promise even greater.
Like President Kennedy challenged the nation before, let this Cancer Moonshot challenge all of us to think anew about what is possible and end cancer as we know it.
It won’t be easy.
But we can do this.
We can give more time.
We can give more hope.
Not someday — but now.
You’ve just read:
Report to the President from the Vice President
Read next:
Report of the Cancer Moonshot Task Force: Executive Summary
Download the Report to the President from the Vice President.